High White Blood Cells? Here's What It Could Mean
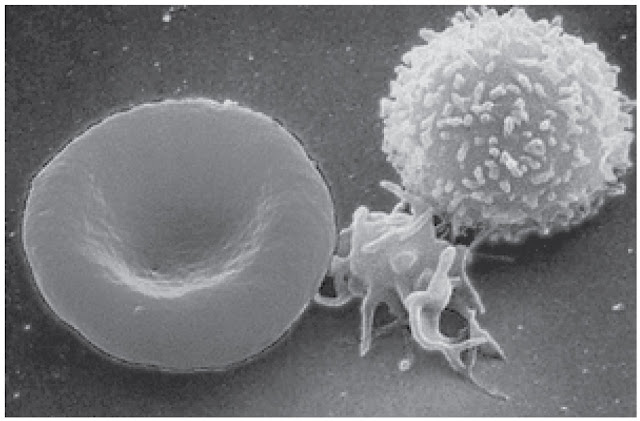
White blood cells (WBCs), also known as leukocytes, are your body’s internal army. Think of them as the bodyguards constantly on the lookout for invaders like bacteria, viruses, fungi, and other harmful substances. Produced primarily in the bone marrow, they are a crucial part of the immune system and are found in your blood and lymphatic system.
There are several types of white blood cells, and each has a unique function:
-
Neutrophils: First responders to bacterial infections.
-
Lymphocytes: Includes T cells and B cells; responsible for targeted immune responses.
-
Monocytes: Clean up debris and turn into macrophages to devour pathogens.
-
Eosinophils: Active during allergic reactions and parasitic infections.
-
Basophils: Involved in allergic responses and inflammation.
Your body normally maintains a balanced WBC count, ensuring you're protected without going into immune overdrive. But when this count rises significantly, it could be a red flag, hinting that something more serious is at play.
Role of WBCs in the Immune System
White blood cells are essential for immune surveillance. They patrol your bloodstream and tissues, searching for signs of trouble. When they detect pathogens or damaged cells, they leap into action—releasing enzymes, engulfing invaders, and calling in reinforcements.
The immune response WBCs trigger is what helps your body fight off illness. However, when this response is overstimulated or out of sync—like during autoimmune diseases or chronic infections—it can lead to persistently high WBC levels, which may be more harmful than helpful.
White blood cells also remember past infections. Lymphocytes, especially memory B and T cells, are why vaccines work. They recall invaders and respond faster the next time you’re exposed.
Normal White Blood Cell Count Range
The typical range for a white blood cell count in adults is between 4,000 to 11,000 cells per microliter of blood. However, this can vary slightly between laboratories due to different testing methods or reference ranges.
Here’s a quick breakdown:
| Age Group | Normal WBC Count (per microliter) |
|---|---|
| Adults | 4,000 – 11,000 |
| Children | 5,000 – 13,000 |
| Infants | 9,000 – 30,000 |
A count above this range is called leukocytosis. But not all increases mean you’re in danger. Sometimes it’s a temporary reaction to something benign—like stress, a minor infection, or even exercise. The key is to understand what’s causing the spike.
What Is Considered a High White Blood Cell Count?
Medical Definition of Leukocytosis
Leukocytosis simply means an elevated white blood cell count. While the term sounds ominous, it isn’t always a sign of a serious problem. The definition typically applies when your WBC count exceeds 11,000 cells per microliter.
There are several subtypes:
-
Neutrophilic leukocytosis: Increase in neutrophils.
-
Lymphocytic leukocytosis: Elevation in lymphocytes.
-
Monocytosis, eosinophilia, and basophilia: When one specific subtype rises disproportionately.
Each subtype can point to different underlying causes. For example, a spike in neutrophils often suggests a bacterial infection, while elevated lymphocytes might be linked to viral infections or even certain cancers.
Different Types of WBCs and Their Functions
Understanding the types of WBCs helps decode what your body is fighting:
-
Neutrophils: The most abundant type, they rush to the site of infection and kill invaders.
-
Lymphocytes: Responsible for adaptive immunity, they include B cells (which produce antibodies) and T cells (which kill infected cells).
-
Monocytes: Become macrophages and digest dead or damaged cells.
-
Eosinophils: Deal with allergens and parasites.
-
Basophils: Release histamine during allergic reactions.
An abnormal increase in any of these can signal a very specific problem. For instance, eosinophilia is often seen in allergic conditions like asthma or parasitic infections.
Ranges That Raise Concern
While a count slightly above normal (say, 12,000–15,000 cells/microliter) might not be urgent, anything over 20,000 warrants a deeper look—especially if it’s persistent. Extremely high WBC counts (above 50,000) are often associated with severe infections, chronic inflammation, or leukemia.
Here’s a general breakdown of when to worry:
-
Mild Elevation (11,000–15,000): Often benign; caused by stress, minor infections, or medications.
-
Moderate Elevation (15,000–30,000): May need further investigation; can indicate infection, inflammation, or immune disorders.
-
High Elevation (30,000–50,000): Could be serious—such as sepsis, leukemia, or autoimmune diseases.
-
Very High (>50,000): Critical and needs immediate attention.
Common Causes of Elevated White Blood Cells
Infections (Bacterial, Viral, Fungal)
One of the most common reasons for a high white blood cell count is an infection. When bacteria, viruses, or fungi invade your body, your immune system kicks into high gear. WBCs multiply rapidly to combat the intruder.
-
Bacterial infections like pneumonia, urinary tract infections, or appendicitis often spike neutrophil levels.
-
Viral infections such as Epstein-Barr virus or hepatitis may raise lymphocyte counts.
-
Fungal infections and parasitic infections can also alter WBC levels, though these are less common.
An important point: WBCs may remain elevated even after the infection resolves. That’s because your immune system takes time to return to baseline.
Inflammatory and Autoimmune Conditions
When your immune system turns against you, as it does in autoimmune diseases, white blood cells increase inappropriately.
Common culprits include:
-
Rheumatoid arthritis
-
Lupus (SLE)
-
Inflammatory bowel disease (IBD)
-
Psoriasis
In these cases, your immune system mistakenly targets your own tissues, causing chronic inflammation. The body responds by releasing more WBCs, especially lymphocytes and monocytes.
It’s also worth noting that inflammatory conditions can cause symptoms that mimic infections—like fatigue, fever, and joint pain—further complicating diagnosis.
Physical and Emotional Stress
Yes, even stress—especially the chronic kind—can elevate your white blood cell count. During periods of high stress, your adrenal glands pump out cortisol, which can mobilize white blood cells into your bloodstream.
-
Physical stressors: surgery, injury, extreme exercise, or burns.
-
Emotional stressors: anxiety, panic attacks, or intense psychological trauma.
This spike is usually temporary. However, if you’re under constant pressure—say from a demanding job or chronic illness—it can lead to prolonged elevation of WBCs and lower immunity.
Serious Conditions Linked to High WBC Count
Leukemia and Other Blood Cancers
This is one of the most concerning causes of high WBC counts. Leukemia is a type of cancer where the bone marrow produces abnormal white blood cells that don’t function properly but keep multiplying.
Types of leukemia include:
-
Acute lymphoblastic leukemia (ALL)
-
Chronic lymphocytic leukemia (CLL)
-
Acute myeloid leukemia (AML)
-
Chronic myeloid leukemia (CML)
These cancers often result in WBC counts well above 50,000, sometimes over 100,000. Other symptoms include fatigue, frequent infections, bruising, and swollen lymph nodes.
Bone Marrow Disorders
Conditions like myeloproliferative disorders cause the bone marrow to produce too many WBCs. These disorders can eventually transform into leukemia.
Examples:
-
Polycythemia vera
-
Myelofibrosis
-
Essential thrombocythemia
In these cases, the problem isn’t infection or inflammation—it’s faulty bone marrow. Diagnosis usually requires a bone marrow biopsy.
Severe Allergic Reactions and Chronic Diseases
Allergic reactions, especially anaphylaxis, can cause spikes in eosinophils and basophils. Chronic diseases like asthma, eczema, or hay fever can lead to mild but persistent WBC elevation.
Other chronic conditions like kidney failure, tuberculosis, or HIV may also alter WBC levels over time.
Symptoms That Indicate a Need for Medical Attention
Fever, Fatigue, and Night Sweats
A white blood cell count that’s too high isn’t usually something you can feel directly—but your body often sends out warning signs that shouldn’t be ignored. Fever is the most common clue. It’s your body's way of saying, “Hey, something’s not right.” When paired with an elevated WBC, a fever often suggests that your body is fighting an infection or inflammation.
Fatigue, another frequent symptom, tends to sneak in slowly. You might chalk it up to a lack of sleep or a busy lifestyle, but when your immune system is overactive, it consumes a lot of energy. That leaves you feeling drained even after a full night's rest. Add night sweats into the mix, and you’ve got a trio of symptoms that definitely warrants a doctor’s visit—especially if they persist for more than a few days.
These signs become more urgent when they occur together or if they appear without an obvious cause. Unexplained fever and fatigue, for instance, could point toward chronic infections, autoimmune diseases, or even cancer. Don’t delay—get checked.
Unexplained Weight Loss
Losing weight without changing your diet or exercise habits might sound appealing at first, but it’s a major red flag when paired with a high WBC count. This isn’t about shedding a few pounds after skipping a couple of meals—it’s usually significant and rapid weight loss, the kind where your clothes start to feel too loose without explanation.
What causes this? Well, your body may be burning more calories fighting off a chronic condition. Or your metabolism may have shifted because of hormonal imbalances or cancerous activity. Conditions like leukemia, lymphoma, or tuberculosis often present with both high white blood cells and unexplained weight loss.
If you’ve dropped more than 5% of your body weight in under six months without trying—and especially if you’re feeling tired or sick—don’t ignore it. It could be your body’s way of waving a red flag.
Swollen Lymph Nodes and Persistent Infections
Swollen lymph nodes are like small alarms under your skin. They usually pop up in the neck, underarms, or groin, and they’re your body’s response to infection. However, if they stay enlarged for weeks, feel firm, or continue to grow, it could signal something more serious.
Persistent infections—like repeated colds, frequent UTIs, or sores that don’t heal—are another sign your immune system is either overworked or not functioning correctly. Your WBC count might be elevated because your body is constantly trying to fend off invaders but not succeeding.
This imbalance between “response” and “resolution” is especially common in chronic illnesses or in cases where the immune system is compromised, like in HIV, autoimmune conditions, or blood cancers. Bottom line? If your body is in a constant cycle of illness and healing, it's time for a deeper look.
How Doctors Diagnose the Underlying Cause
Complete Blood Count (CBC) and Differential
The first step in diagnosing elevated white blood cells is a Complete Blood Count (CBC). It’s a simple, fast blood test that measures the total number of white blood cells and gives a breakdown of each type.
Here’s what the test typically includes:
-
WBC total count
-
WBC differential (neutrophils, lymphocytes, monocytes, eosinophils, basophils)
-
Hemoglobin and hematocrit
-
Red blood cell count
-
Platelet count
The differential is especially useful. For instance, high neutrophils might mean a bacterial infection, while high lymphocytes could point to a viral infection or certain cancers. This breakdown helps doctors narrow down the possibilities and decide if further testing is needed.
Additional Blood Tests and Imaging
If your WBC count is consistently high or rising rapidly, doctors won’t stop at just a CBC. Depending on your symptoms, they may order:
-
CRP and ESR tests (to check for inflammation)
-
Blood cultures (to detect infections)
-
Liver and kidney function tests
-
Autoimmune panels
-
HIV, hepatitis, or tuberculosis tests
Imaging studies like X-rays, CT scans, or MRIs may also be recommended, especially if there's suspicion of hidden infections, tumors, or organ damage. For example, if you have chest pain and high WBCs, a chest X-ray can reveal pneumonia or lung tumors.
Bone Marrow Biopsy and Genetic Testing
When initial tests raise red flags for serious disorders—particularly blood cancers or bone marrow diseases—a bone marrow biopsy is often the next step. This procedure involves removing a small sample of bone marrow, usually from the hip bone, to examine under a microscope.
Doctors use this to check for:
-
Leukemia
-
Lymphoma
-
Myelodysplastic syndromes
-
Myeloproliferative neoplasms
In some cases, genetic testing may also be conducted to identify mutations or chromosomal abnormalities linked to cancer or inherited conditions. These in-depth tests help doctors decide on targeted therapies or specialized treatments.
When to Seek Immediate Medical Help
Sudden Spike in WBCs
If your WBC count jumps dramatically in a short period—especially with no clear infection—it’s time to take action. A sudden spike can be your body’s response to acute inflammation or a rapidly developing disease, like sepsis or acute leukemia.
Here are some signs that accompany an emergency-level WBC elevation:
-
Sudden, high-grade fever (above 103°F)
-
Confusion or disorientation
-
Rapid heart rate or low blood pressure
-
Difficulty breathing
This isn’t a wait-and-see situation. A sudden surge in white blood cells with these symptoms could mean your body is overwhelmed. Immediate hospitalization may be necessary.
Accompanying Alarming Symptoms
Even if your white blood cell count isn’t sky-high, certain symptoms make it clear that you need urgent medical attention:
-
Chest pain or tightness
-
Shortness of breath
-
Severe headache or visual disturbances
-
Seizures
-
Uncontrolled bleeding or bruising
These could indicate conditions like blood clots, stroke, or hemorrhagic complications, all of which may be linked to or worsened by abnormal white cell activity.
Monitoring WBC Trends Over Time
Sometimes, a single test doesn’t tell the whole story. That's why doctors look at WBC trends over time. Are the numbers rising steadily? Do they spike and then return to normal? Are they associated with new or worsening symptoms?
Keeping track of these trends can help differentiate between temporary spikes (like those caused by stress or infection) and chronic elevations that suggest something deeper. Your healthcare provider may recommend repeat CBCs every few weeks or months depending on the context.
This is especially critical if you’re being treated for a chronic illness, are on immunosuppressants, or have a family history of blood disorders.
Treatment Options Based on Diagnosis
Antibiotics for Infections
If your elevated white blood cell count is due to a bacterial infection, the first line of defense is often antibiotics. These medications target and kill bacteria, helping your body recover and bringing your WBC count back to normal.
Doctors usually prescribe antibiotics based on:
-
The type of infection (e.g., respiratory, urinary, skin)
-
The severity of your symptoms
-
Culture results, if available (to identify the specific bacteria)
In most cases, your WBC count will start to decrease as the infection clears. But it’s important to finish the full course of antibiotics—even if you start feeling better early on. Cutting it short could cause the infection to come back stronger or become resistant to treatment.
In more serious infections, such as pneumonia, sepsis, or abscesses, hospitalization and intravenous (IV) antibiotics may be necessary. Delayed treatment can be dangerous, especially in people with weakened immune systems.
Immunosuppressants for Autoimmune Diseases
When your elevated white blood cells are due to an autoimmune condition like lupus, rheumatoid arthritis, or inflammatory bowel disease, the goal is to reduce immune system overactivity. That’s where immunosuppressant drugs come in.
Common options include:
-
Corticosteroids (like prednisone)
-
Methotrexate
-
Biologic agents (such as TNF inhibitors)
-
Cyclophosphamide or azathioprine
These medications don’t just suppress symptoms—they lower inflammation and help normalize WBC levels by dialing down immune system activity. However, they do come with side effects, such as a higher risk of infections or liver toxicity, so they require careful monitoring.
Treatment is typically ongoing and adjusted over time. Your doctor will track your blood counts, symptoms, and side effects to find the safest and most effective balance.
Chemotherapy or Targeted Therapy for Cancer
If your high WBC count is due to a blood cancer like leukemia, more aggressive treatment is needed. This might include:
-
Chemotherapy: Uses powerful drugs to kill rapidly dividing cancer cells.
-
Targeted therapy: Blocks specific genes or proteins involved in cancer growth (e.g., tyrosine kinase inhibitors for chronic myeloid leukemia).
-
Immunotherapy: Stimulates your immune system to attack cancer cells.
-
Bone marrow transplant: Replaces diseased marrow with healthy stem cells.
Cancer treatment often involves a team of specialists, including oncologists, hematologists, and support staff. The journey can be long, but many blood cancers are now highly treatable, especially when caught early.
Side effects of treatment, like fatigue, infections, or hair loss, are common—but manageable with the right care and support. Monitoring WBCs regularly during and after treatment is key to tracking progress and spotting relapses early.
Natural Ways to Maintain a Healthy WBC Count
Diet and Nutrition
Your immune system needs the right fuel to function properly, and that includes maintaining a balanced white blood cell count. A diet rich in antioxidants, vitamins, and minerals can help your body fight off infections and inflammation naturally.
Here’s what to eat more of:
-
Leafy greens: Spinach, kale, and broccoli are rich in vitamin C and folate.
-
Citrus fruits: Oranges, lemons, and grapefruits boost immunity.
-
Nuts and seeds: Almonds and sunflower seeds provide vitamin E and zinc.
-
Garlic and onions: Natural antimicrobial properties.
-
Fermented foods: Yogurt, kefir, and kimchi promote gut health.
On the flip side, try to avoid processed foods, excessive sugar, and trans fats, as these can trigger inflammation and weaken your immune system.
Drinking plenty of water, avoiding alcohol, and limiting caffeine also help maintain a healthy blood environment.
Stress Reduction and Sleep
Chronic stress is a silent immune system killer. When you're stressed, your body produces cortisol, which can cause your WBC levels to spike temporarily but weaken their effectiveness over time. That’s why managing stress isn’t just good for your mental health—it directly affects your white blood cells.
Simple ways to reduce stress include:
-
Meditation or deep breathing
-
Journaling or gratitude practice
-
Spending time in nature
-
Listening to calming music
-
Setting boundaries at work and home
And don’t forget sleep. Aim for at least 7–9 hours of uninterrupted sleep per night. Your body repairs itself during sleep, and poor sleep quality has been linked to weakened immunity and higher inflammation levels.
Regular Exercise and Immune Support
Moderate, consistent exercise is one of the best ways to keep your immune system humming and your WBCs in balance. Activities like walking, swimming, or yoga help improve circulation, reduce stress, and enhance immune cell function.
However, too much intense exercise—like marathon training or heavy lifting every day—can have the opposite effect. It may cause temporary WBC spikes or even suppress immune activity.
Striking a healthy balance is key. Aim for:
-
150 minutes of moderate activity per week
-
Strength training two times a week
-
Stretching and mobility exercises to reduce injury risk
You can also consider natural supplements (with a doctor’s approval), such as:
-
Vitamin D
-
Zinc
-
Elderberry
-
Probiotics
These can support immune function and help regulate inflammation that might otherwise elevate WBC counts.
Monitoring Your White Blood Cell Count
Regular Blood Tests
Monitoring your WBC count isn’t a one-and-done thing. If you’ve ever had a high count, your doctor may recommend routine blood work to keep tabs on any fluctuations or emerging patterns.
Depending on your health status, you might get tested:
-
Monthly (if you’re undergoing treatment or being closely monitored)
-
Every 3–6 months (for chronic conditions)
-
Annually (for general wellness)
Keeping your test results in a personal health journal or app can help you spot trends and ask smarter questions during doctor visits.
Tracking Symptoms and Changes
Your body often tells you what’s going on—if you’re listening. Keep an eye on:
-
Energy levels
-
Appetite and weight
-
Frequency of infections
-
Skin changes (rashes, bruises, swelling)
Documenting these changes in a health diary or on your phone can be incredibly helpful, especially if your symptoms come and go. Share this information with your doctor to help guide your care plan.
Communicating With Your Healthcare Provider
Your doctor is your partner in health, and keeping an open line of communication is essential. Don’t be afraid to ask:
-
What does my WBC count mean in my case?
-
Do I need more tests?
-
Is this a one-time spike or something chronic?
-
What symptoms should I watch for?
-
When should I seek emergency care?
Having a clear understanding of your lab results and a personalized follow-up plan can help you feel more in control of your health journey.
Living With a Chronic Condition That Affects WBCs
Autoimmune Diseases Management
If you’re living with an autoimmune disease, keeping your white blood cell count within a safe range becomes part of your everyday routine. Conditions like lupus, rheumatoid arthritis, multiple sclerosis, and Crohn’s disease cause your immune system to become hyperactive, leading to elevated WBC levels.
Managing these conditions usually involves a combination of:
-
Medication: Immunosuppressants or corticosteroids help tone down the immune response.
-
Lifestyle changes: Anti-inflammatory diets, exercise, and sleep hygiene.
-
Regular check-ups: Routine blood tests to monitor WBC trends and medication effects.
Flare-ups are part of life with autoimmune diseases, but recognizing your triggers—stress, poor diet, lack of rest—can reduce their frequency. Keeping a symptom journal helps you stay one step ahead of potential issues.
Support groups and therapy can also play a huge role. Living with a chronic condition can be mentally taxing, but connecting with others in the same boat provides both comfort and practical tips.
Cancer Survivorship
For cancer survivors, especially those who’ve battled leukemia or lymphoma, WBC management is a long-term concern. Even after treatment, your immune system might remain fragile or behave unpredictably.
You may experience:
-
Lower-than-normal WBCs (leukopenia) from chemotherapy.
-
Delayed immune responses to infections or vaccinations.
-
Post-treatment fatigue and vulnerability to illness.
To navigate survivorship safely, your healthcare team may recommend booster shots, antiviral medications, or nutritional support. Regular follow-ups are essential—not just for cancer recurrence, but for immune health monitoring too.
Remember, survivorship isn’t just about surviving—it’s about regaining quality of life. Stay engaged with your health team and advocate for a plan that works for your lifestyle and long-term well-being.
Managing Risk Factors Proactively
You can’t always control why your white blood cells spike, but you can reduce the risk of dangerous elevations by managing contributing factors. Focus on:
-
Controlling blood sugar (diabetes can lead to chronic inflammation)
-
Quitting smoking (which increases WBC count)
-
Limiting alcohol (excessive use suppresses immune function)
-
Maintaining a healthy weight (obesity is linked to systemic inflammation)
By addressing these risk factors, you’re helping your immune system stay in balance—and improving your overall health in the process. Prevention is a powerful tool, and even small daily changes can make a big difference.
Myths and Misconceptions About High WBC Count
WBC Elevation Always Means Cancer
Let’s bust one of the most common fears: an elevated white blood cell count doesn’t automatically mean cancer. Sure, leukemia and lymphomas can cause high WBCs, but the majority of elevated counts are due to far more common reasons, like infections, inflammation, or stress.
Cancer is usually diagnosed based on a combination of factors—not just a single lab result. These include symptoms, imaging, biopsy results, and ongoing trends. So while a high count might be a reason for further testing, it’s not a verdict by itself.
Natural Remedies Can Replace Medical Treatment
While natural remedies and lifestyle changes can help support your immune health, they’re not substitutes for medical treatment. Herbal teas, vitamin C, or turmeric may ease inflammation, but they won’t cure an infection or treat leukemia.
Relying solely on natural methods—especially for serious conditions—can delay proper treatment and lead to complications. Always discuss supplements or alternative therapies with your doctor before trying them.
WBC Count Is the Only Marker of Illness
White blood cells are just one piece of the puzzle. A high WBC count doesn’t always indicate how severe your illness is, nor can it reveal the exact cause on its own.
Doctors use a range of other indicators to evaluate your health:
-
C-reactive protein (CRP)
-
Erythrocyte sedimentation rate (ESR)
-
Imaging studies
-
Symptom history
-
Other blood markers (platelets, red cells, hemoglobin)
Focusing solely on WBC count without context can lead to unnecessary worry. Trust your doctor to interpret the full picture.
Preventive Measures for White Blood Cell Health
Vaccinations and Infection Prevention
Staying up to date on vaccinations is a frontline defense in keeping your white blood cell count in check. Vaccines help your immune system prepare for future encounters with viruses like:
-
Influenza
-
COVID-19
-
Hepatitis B
-
Pneumonia
-
Shingles
They also reduce the chances of your immune system being caught off guard—which means fewer spikes in white blood cells due to infection. Good hygiene also plays a major role in prevention:
-
Wash hands regularly
-
Avoid close contact with sick individuals
-
Clean surfaces and shared items
-
Practice safe food handling
Prevention isn’t always glamorous, but it’s powerful.
Healthy Lifestyle Choices
You’ve heard it a million times—but diet, sleep, exercise, and mental well-being genuinely affect your immune system and white blood cell production. Here’s your wellness checklist:
-
Eat a balanced diet rich in whole foods
-
Get 7–9 hours of quality sleep per night
-
Exercise moderately at least 3–5 times per week
-
Avoid smoking and limit alcohol intake
-
Stay mentally active and manage stress
Your lifestyle is the long-term solution that keeps your WBC count balanced and your immune system efficient.
Early Detection and Screening
Routine health screenings are essential—even if you feel fine. Periodic CBCs, physicals, and check-ins with your healthcare provider can catch imbalances before they become serious.
If you have a family history of blood disorders or autoimmune diseases, your doctor may recommend more frequent monitoring. Early intervention leads to better outcomes—plain and simple.
Talking to Your Doctor About White Blood Cell Results
Questions to Ask
When reviewing your blood test results, don’t be shy. Here are a few smart questions to bring to your next appointment:
-
What does my elevated WBC count mean?
-
Could this be due to a recent illness or medication?
-
Do I need additional tests or imaging?
-
Should I be concerned about cancer?
-
What are the next steps?
Being proactive with your questions builds a more informed and collaborative relationship with your doctor.
Understanding Your Blood Test Reports
Blood test reports can be confusing, full of abbreviations and numbers. Here’s a simple key to interpret the WBC portion:
-
WBC: Total white blood cells
-
NEUT: Neutrophils
-
LYMPH: Lymphocytes
-
MONO: Monocytes
-
EOS: Eosinophils
-
BASO: Basophils
If anything’s marked “high” or “low,” it doesn’t always mean danger. But it does mean it’s worth asking about—especially if paired with symptoms.
Building a Long-Term Health Plan
Whether your WBC count is slightly elevated or dangerously high, it’s essential to look at the bigger picture. Work with your doctor to create a personalized health plan that may include:
-
Lifestyle adjustments
-
Medication or supplements
-
Routine blood tests
-
Chronic condition management
-
Preventive screenings
Think of it like a roadmap—guiding you to better health and helping you avoid unnecessary detours or breakdowns.
Conclusion
A high white blood cell count can be caused by something as simple as stress or as serious as cancer. The key is understanding what your body is trying to tell you. Paying attention to your symptoms, getting regular check-ups, and working closely with your healthcare provider can help you catch issues early, manage chronic conditions, and maintain overall wellness.
Don’t panic when you see a high number—investigate, monitor, and take proactive steps. Your immune system is your best line of defense. Treat it well, and it’ll take care of you.
FAQs
1. Can stress cause a high white blood cell count?
Yes, both physical and emotional stress can temporarily elevate your WBC count by releasing cortisol and other stress hormones.
2. Is a high WBC count always serious?
Not always. It could be a response to infection, inflammation, or even exercise. But persistent or extremely high levels should be evaluated.
3. What foods help regulate WBC count?
Leafy greens, citrus fruits, nuts, seeds, fermented foods, and garlic all support immune balance and healthy WBC production.
4. How often should I get my WBC checked?
If you're healthy, annually is fine. For chronic conditions or abnormal results, your doctor may recommend more frequent testing.
5. Can exercise affect my white blood cell count?
Yes, intense exercise can temporarily increase WBC levels, but regular moderate activity supports overall immune health.